Abstract
Introduction
Sickle cell disease (SCD) is the most common inherited blood disorder in Jamaica. SCD is associated with significantly shortened lifespans globally. SCD has serious health complications and individuals with SCD often experience poor quality of life (QoL) and high levels of perceived stigma as a result. Stigma acts as a barrier to self-management, and affects morbidity, mortality, and QoL in individuals with SCD. Sources and perceptions of stigma depend largely on culture, society, and environment. The purpose of this study is to describe health-related QoL, perceived stigma, and measure the relationships between these concepts in adults with SCD in Jamaica.
Methods
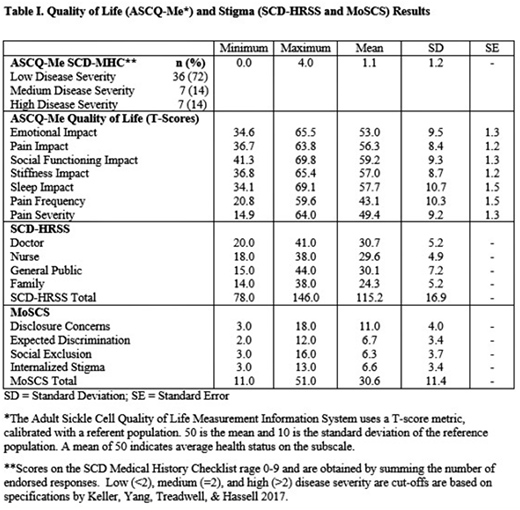
Inclusion criteria were >18 years of age and self-reported diagnosis of a SCD genotype. Participants were recruited from the Sickle Cell Unit at The University of the West Indies in Kingston, Jamaica. Participants (n=50) completed interviewer-administered surveys including demographic/clinical characteristics; SCD Health Related Stigma Scale (SCD-HRSS) subscales: family, general public, doctors, nurses (scores range 10-60, total 40-240); the Measure of Sickle Cell Stigma (MoSCS) subscales: disclosure concerns, expected discrimination, social exclusion, internalized stigma (scores range 3-18, 2-12, 3-18, 3-18 respectively; total 11-66); and the Adult Sickle Cell Quality of Life Measurement System (ASCQ-Me) subscales: Emotional Impact, Sleep Impact, Social Functioning Impact, Stiffness Impact, Pain Impact, and Pain Episode Frequency and Severity. ASCQ-Me uses a T-score metric where 50 is the mean of the reference population and 10 is the standard deviation. The value of 50 indicates the health score of the average field test respondent during testing of the ASCQ-Me in the United States. Higher scores indicate healthier status for all subscales except pain episode frequency and severity. Scores were determined by using the online scoring system at Healthmeasures.net as recommended. The MoSCS and SCD-HRSS are both scored by obtaining summing the mean score of the subscales; higher scores indicate higher perceived stigma. Descriptive statistics were used to report scores per subscale. To identify a relationships between QoL and stigma a set of Spearman point-biserial correlation analyses were performed.
Results
Fifty individuals (average age 34.4 +/- 11.4; 94% Black) were recruited, 22 (44%) males and 28 (56%) females. The majority of the sample reported low disease severity. Participants reported average to healthier status on the ASCQ-Me domain in comparison to the normative United States population. Low to moderate levels of stigma were reported. See Table I for ASCQ-Me, SCD-HRSS, and MoSCS results. There were weak but significant relationships identified between the QoL measures and the stigma scales, according to the lenient p ≤0.10 significance level that was used for this exploratory study. A positive correlation was identified between pain frequency and stigma (SCD-HRSS: r=0.303, p: 0.043; MoSCS: r=0.379 p: 0.008), indicating that individuals who report experiencing more frequent pain may also report higher stigma. Negative correlations were identified between stigma and both emotional impact (SCD-HRSS: r=-0.335, p=0.025; MoSCS: -0.331, p=0.021) and social functioning (MoSCS: r=-0.397; p=0.005); suggesting that individuals who report less emotional impact, as a result of having SCD, and better social functioning also experience less perceived stigma.
Conclusion
It is important to note that while participants in this Jamaican sample of adults with SCD reported average to healthier status on the QoL measures than the normative population of individuals with SCD, this does not signify better QoL than the general population. A previous study found that in comparison to the general population, individuals with SCD reported QoL levels most similar to those undergoing hemodialysis. Our sample reported low levels of stigma, which is also consistent with also having lower disease severity. Correlational analysis revealed relationships that indicate that greater disease severity (pain frequency) could result in higher stigma levels, while experiencing less psychosocial (social functioning and emotional) impacts could result in lower stigma levels.
Bulgin:NIH NINR: Research Funding; Jonas Nurse Leaders Scholar Program: Other: Education Funding ; Duke Global Health Institute Field Work Grant: Research Funding. Tanabe:Alliant Health: Consultancy; NIH and AHRQ: Research Funding; Duke University: Employment.
Author notes
Asterisk with author names denotes non-ASH members.